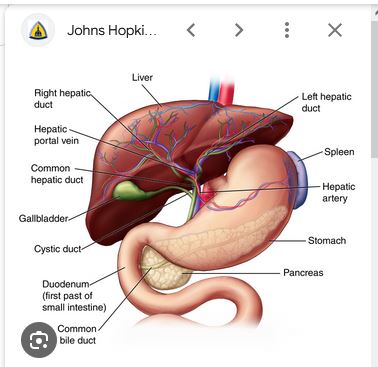
What is it?
Primary Sclerosing Cholangitis is a progressive autoimmune disease that slowly destroys the bile ducts (which drain bile fluid from the liver). This leads to liver failure and eventually to death or (if lucky) a liver transplant. The fact that I am typing this tells you that I fall into the latter category! But I know five people personally–Sandi, Tim, Arne, Melanie, Jutta–who didn’t make it, including the young lady to my left in the photo below. Either they did not get the organ in time or they were too sick to undergo the transplant. (For that matter, I also almost didn’t make it myself when my MELD score got up to 27 but I was too sick to be transplanted.)

What is the time frame?
PSC can take a long time to develop (20 years), but when it gets to the serious stage it is SERIOUS! On the positive side: Social Security Disability Insurance (SSDI) was practically automatic. However, getting on Medicare took longer, but I was saved by the ACA in the interim.
What are the symptoms?
- Severe itching all over the body
- Chills, even under a hot shower
- Pale stools and dark urine (sorry if TMI)
- Jaundice (especially the eyes)
- Pancreatitis (I escaped that one)
- Chronic fatigue
- Esophageal varices (in throat)
- Brain fog (hepatic encephalopathy)
- Not allowed to drive a car
- Fluid retention due to portal hypertension (ascites)
- Terrible leg cramps
- Tooth decay
- Foul breath (fetor hepaticus)
- Inguinal hernia
- Occasional need for wheelchair or walker
- Associated ulcerative colitis
- Progression to liver cancer
- (And more)
What can be done about it?
There are medications and procedures that alleviate some of the symptoms and prolong the time until transplant, but there is (as of yet) no cure.
Who advocates for PSC research?

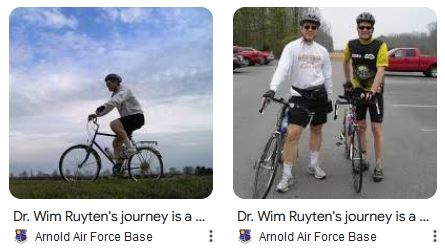
PSC is an orphan disease. But there is a fantastic organization that advocates for more research: Partners Seeing a Cure (see https://pscpartners.org/). I once (in 2009, when I was still strong enough) rode my bicycle 512 miles from Tullahoma to Chicago to support a PSC fundraiser (see also pic above). You can still read about that at https://www.arnold.af.mil/News/Features/Display/Article/410637/dr-wim-ruytens-journey-is-a-ride-for-life/.
The waiting list
Yes, there is a waiting list for organ transplants. In the case of livers, you have to be very sick (as measured by the so-called MELD score–mine got up to 27 a few times) to qualify. I was on the list for three-and-a-half years, until I got “the call” on December 2, 2020: “How soon can you be here?” (My doctor expected me to be transplanted 4-6 months from being listed–not an easy wait.)
My transplant
I had my transplant at Vanderbilt University Medical Center, in the wee hours of December 3rd, 2020, with Dr. Geevarghese attending (https://www.vumc.org/surgical-sciences/person/sunil-k-geevarghese-md-msci-facs). I will be forever grateful to VUMC, in particular to my hepatologist of 20 years, Dr. David Raiford (now retired). Needless to say, I am also very much thankful to the (anonymous) family that decided to donate the organ from their deceased son. Also, I consider myself doubly lucky: Not only was I able to have the transplant, but the cancer spots on my old liver had not metastasized.
P.S.: My new liver was Hepatitis-C positive initially, but medication nixed that in about a one-month period!

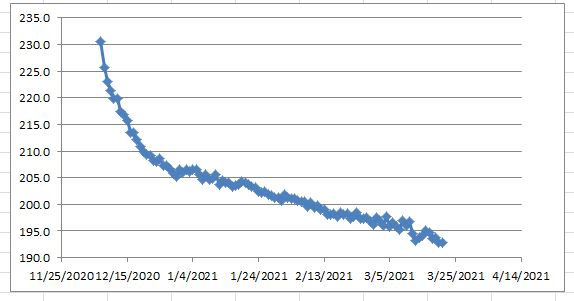
In the picture I still have the fluid build-up in my body–I lost 40 lbs in three months since my transplant, as shown in the chart below (for fellow nerds: exponential decay followed by linear decay). I was lucky in that I never required paracentesis (periodic fluid removal), as some patients do.
Cost of transplant
In excess of $625,000 billed (of which I only paid a small portion). Thank you Humana for taking care of me! Also for providing, free of charge, a clinical consultant to keep tabs on my progress from time to time.
Post transplant
It was striking: I already felt so much better the very next day, as the fog had cleared from my head. But to be frank, it has taken me several years to regain my vitality. Lately I feel like I have awakened from a long dream, and I am ready do reengage in aspects of life that I had kept on the back burner. Hence this blog 🙂
Continued medication and diet

Transplant patients have to take anti-rejection medication for the rest of their lives (in my case, Tacrolimus and Mycophenelate Mofetil–see pic). This is hard on the kidneys, and I have to follow a low-potassium diet (no white potatoes, no bananas, no watermelon, limited tomatoes). Also, I have to wear sunscreen more urgently than a normal person and I have to drink lots of water. Finally, I have minor balance issues from the medication I have to take.
Further transplants?
Some unlucky patients will eventually require a kidney transplant in addition to their liver transplant, as a result of having to take the anti-rejection medication. It is also possible that PSC will return in the new liver, requiring a subsequent liver transplant. But as of now, routine bloodwork shows that my new liver is happy, and my kidneys are just a little bit bad. I hope to keep it that way!